New Tampa Bay Health Alliance aims to restore doctor-patient relationships
The network, called the Tampa Bay Health Alliance, will include the USF Physicians Group and four other practices with various specialties and primary care — Florida Medical Clinic, Florida Orthopaedic Institute, Pediatric Health Care Alliance and Women’s Care Florida.
What some experts call the wave of the future in health care, and an attempt to restore the traditional doctor-patient relationship as its core, is coming to the Tampa Bay area.
Partly at the instigation of the University of South Florida, a group of five large, local physician practices are announcing formation of what’s called a “clinically integrated network” to care for patients.
The network, called the Tampa Bay Health Alliance, will include the USF Physicians Group and four other practices with various specialties and primary care — Florida Medical Clinic, Florida Orthopaedic Institute, Pediatric Health Care Alliance and Women’s Care Florida.
The five total more than 1,300 health care professionals with more than 750,000 patients and scores of locations throughout the Tampa Bay region.
For patients, the organization means they eventually could receive virtually all their health care through a single network with shared records and appointment services.
Ultimately, say health care experts, the formation of such networks could lead to major changes in how health care is provided.
Restoring doctor-patient relationships
Some hope physician-based networks of this kind will restore the primacy of the doctor-patient relationship, and possibly decrease or even eliminate the role of insurance companies in paying for and regulating health care.
Some of those changes may lie in the future, but the immediate goal of the Tampa Bay Health Alliance will be to provide consumers “a smoother customer experience,” says Daniel Vukmer, an associate VP at USF Health and associate dean of the USF medical school.
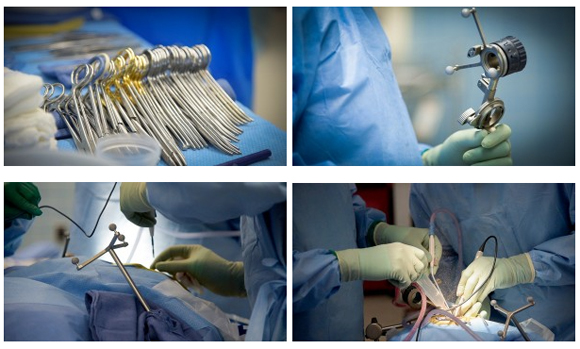
He says that entails greater efficiency, lower costs and smoother transitions from one phase of care to another – consultation, testing, imaging, and prescribing or procedures.
By the time Vukmer arrived at USF in January, he says, the CEOs of the five physician practices involved had already started negotiations for the project. Vukmer, 54, a Pennsylvania native who went to Juniata College and Delaware’s Widener University law school, was brought in to formally launch it and will be its CEO.
He has worked with similar networks at Ohio State University and University of Pittsburgh Medical Center, but says this project is a kind that’s unique in the Tampa Bay area, rare nationwide and the first of its kind he has worked in – a physician-led clinically integrated network, as opposed to one run by a hospital or hospital group.
In Pittsburgh, according to USF Health’s website, Vukmer helped develop one of the largest provider-owned health plans in the United States, with some 2 million patients.
“Many networks across the country call themselves integrated networks, but they’re not fully integrated,” he says. “We’re not fully integrated yet either, but that is the goal.”
“Fully integrated,” he says, would mean coordinating appointments, medical records and medical protocols for all patients, possibly hiring care coordinators to manage each case and pharmacists to dispense prescriptions.
Initially, the network’s patients won’t see a big difference in how they access health care.
“You’ll still be buying your insurance policy or using your employee plan, taking your card to your doctor’s office,” he says. The network hopes to contract with insurance companies and employers with self-funded health plans.
“What we hope will change is that by sharing records and other data, we can avoid duplicative tests and duplicative imaging, and avoid drug interactions. By communicating and being integrated with different groups, handoffs or transitions of care can be smoother.”
Ultimately, he says, the network could develop coverage products to be sold directly to consumers, replacing their insurance policies.
Similar networks already exist
Tampa Bay Health Alliance isn’t the first clinically integrated network in the Tampa Bay area, and it probably won’t be the last.
The largest is Baycare, a non-profit group that owns 14 hospitals plus urgent care centers, and includes a clinically integrated network, Baycare Physician Partners, whose website boasts 1,380 physicians in 600 practices.
Baycare’s network is larger and four years old, but it doesn’t yet have the integration features Vukmer said he hopes to develop at Tampa Bay Health Alliance, including common medical records and scheduling, says its Clinical Performance Director, Physician Eli Freilich.
But Freilich says his organization is “physician-led” – its CEO and nearly all its board of directors are physicians.
Tampa General Hospital, which already has an alliance with Florida Hospital, is also working on forming what it calls “a similar network.”
“We think this new alliance is a positive development for Tampa Bay residents,” TGH spokesman John Dunn says of the Tampa Bay Health Alliance. “It will combine the clinical strengths of these organizations to provide more efficient, high quality care, and also expand their reach further into the communities they serve.”
TGH expects to work with the new alliance because it already has relationships with some of the organizations involved.
But Vukmer said Tampa Bay Health Alliance is unique because it consists solely of physician practices.
“The decisions are made entirely by physicians,” he says. “We have the motive of keeping patients healthy and keeping them out of the hospital, not putting them in the hospital.”
Most clinically integrated networks are led by hospitals or health systems.
“From my experience in several different markets, this could be one of the largest of its kind in the country.”
Rebuilding a sacred trust
Jay Wolfson, public health professor at USF, says clinically integrated networks are in part a response to changes in health care brought about by the Affordable Care Act, sometimes called Obamacare, and by the push for greater efficiency and lower costs under Medicare.
The Affordable Care Act and the federal Center for Medicare and Medicaid Services have sought to create efficiencies by encouraging various parts of the medical community to work together and by encouraging health care plans that reimburse practitioners based on outcomes – on the patient’s health rather than on procedures performed.
For several decades, Wolfson says, health care professionals have bemoaned the gradual fracturing of what they call the “sacred trust” between patient and physician, as hospitals and insurance companies apply more and more restrictions on medical practice.
“Physicians have been picked off one at a time by larger organizations because they haven’t been a cohesive group,” he says.
That makes it significant that this network is being formed by physicians.
“A hospital is a building, and an insurance company is basically a bank. They don’t provide you with care. This keeps it closer to that direct clinical relationship between the physician and the patient or family,” Wolfson says.
Vukmer agrees that the Affordable Care Act and Medicare are part of the cause of the movement toward health care networks, but says this kind of change would have been coming anyway.
“Whether we like the ACA or don’t like it, the reality is it started the industry to think about making these kinds of changes, being more efficient and consumer-centric,” he says. “It doesn’t matter at this point who’s president or what the law is – there have been wheels set in motion that consumers want better access and lower prices.”